Summary: Researchers have successfully used a custom-made robot to treat wet age-related macular degeneration (AMD). This minimally invasive treatment reduces the need for frequent eye injections.
The landmark study found that robotic radiotherapy significantly reduces the number of injections needed, potentially saving millions of dollars each year. The new method provides precise targeting of radiation to the eye, improving patient outcomes and reducing costs.
Highlights:
- The new robotic system reduces the need for frequent eye injections in AMD patients.
- Robotic radiotherapy provides precise and targeted treatment, thereby reducing disease activity.
- The study predicts significant savings for the NHS, reducing the treatment burden on patients.
Source: King’s College London
King’s researchers and doctors from King’s College Hospital NHS Foundation Trust have successfully used a new robotic system to improve the treatment of debilitating eye diseases.
The custom-built robot was used to treat wet neovascular age-related macular degeneration (AMD), delivering a single, minimally invasive dose of radiation, followed by routine treatment of patients with injections into the eye .
In the landmark essay, published today in The LancetIt was found that patients then needed fewer injections to effectively control the disease, saving around 1.8 million injections per year worldwide.
Wet AMD is a debilitating eye disease in which new abnormal blood vessels develop in the macula, the layer of light-detecting cells at the back of the eyeball. The vessels then begin to leak blood and fluid, usually causing rapid, permanent, and severe vision loss.
Worldwide, around 196 million people suffer from AMD and the Royal College of Ophthalmologists estimate that the condition affects more than 700,000 people in the UK. The number of people with AMD is expected to increase by 60% by 2035, due to the country’s aging population.
Wet AMD is currently treated with regular injections into the eye. Initially, the treatment significantly improves the patient’s vision. But because injections don’t cure the disease, fluid will eventually start to build up in the macula again and patients will need repeated, long-term injections.
Most people need an injection around every 1 to 3 months, and eye injections, costing between £500 and £800 per injection, have become one of the most common procedures in the NHS.
The new treatment can be much better targeted than existing methods, by directing three highly focused beams of radiation toward the diseased eye. Scientists found that patients receiving robotic radiotherapy needed fewer injections to control their disease compared to standard treatment.
The study found the robot-controlled device saves the NHS £565 for every patient treated in the first two years because it results in fewer injections.
Study leader and first author of the paper, Professor Timothy Jackson, of King’s College London and consultant eye surgeon at King’s College Hospital, said: “Research has already attempted to find a better way to target the radiotherapy on the macula, for example by reusing used devices. to treat brain tumors. But until now, nothing has been precise enough to target macular disease that can measure less than 1 mm in diameter.
“With this specially designed robotic system, we can be incredibly precise, using overlapping beams of radiation to treat a very small lesion at the back of the eye.
“Patients generally accept that they need to have eye injections to preserve their vision, but frequent hospital attendance and repeated eye injections are not something they enjoy. By better stabilizing the disease and reducing its activity, the new treatment could reduce the number of injections needed by about a quarter. Hopefully, this discovery will reduce the treatment burden that patients have to bear.
Dr Helen Dakin, research lecturer at the University of Oxford, said: “We found that the savings from fewer injections are greater than the cost of robot-controlled radiotherapy. This new treatment can therefore save the NHS money which can be used to treat other patients, whilst controlling patients’ AMD as well as standard care.
Funding: The research was jointly funded by the National Institute for Health and Care Research (NIHR) and the Medical Research Council (MRC) and recruited 411 participants across 30 NHS hospitals. A commentary commissioned by the Lancet and accompanying the article described it as a “historic trial”.
This study was led by researchers from King’s College London and doctors from King’s College Hospital NHS Foundation Trust, in collaboration with the University of Oxford, the University of Bristol and Queen’s University Belfast.
About this research news in robotics and visual neuroscience
Author: Rebecca Lewis
Source: King’s College London
Contact: Rebecca Lewis – King’s College London
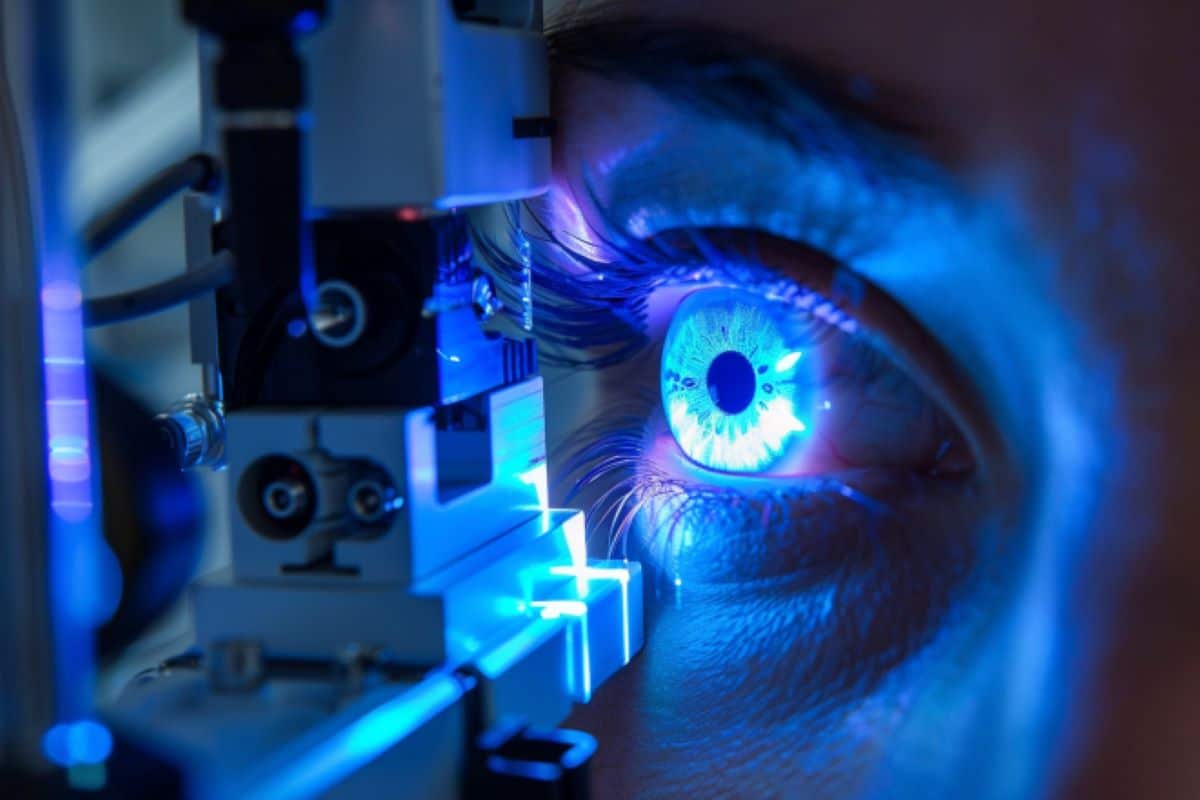
Picture: Image is credited to Neuroscience News
Original research: Free access.
“Stereotactic radiotherapy for neovascular age-related macular degeneration (STAR): a pivotal, randomized, double-blind, sham-controlled trial” by Timothy Jackson et al. The Lancet
Abstract
Stereotactic Radiotherapy for Neovascular Age-Related Macular Degeneration (STAR): A Pivotal, Randomized, Double-Blind, Sham-Controlled Trial
Background
Neovascular age-related macular degeneration (AMD) is a leading cause of blindness. First-line treatment consists of anti-vascular endothelial growth factor (anti-VEGF) agents administered by intravitreal injection. Ionizing radiation attenuates the main pathogenic processes underlying AMD and therefore has therapeutic potential.
STAR aimed to evaluate whether stereotactic radiotherapy (SRT) reduced the number of anti-VEGF injections needed, without sacrificing visual acuity.
Methods
This pivotal, randomized, double-blind, sham-controlled trial recruited participants with pretreated chronic active AMD from 30 UK hospitals. Participants were randomly assigned in a 2:1 ratio to receive 16-Gray (Gy) SRT delivered using a robot-controlled device or sham SRT, stratified by treatment center.
Eligible participants were aged 50 years or older and had chronic active AMD, with at least three prior anti-VEGF injections, including at least one in the past 4 months. Participants and all trial and image reading center staff were masked to treatment allocation, with the exception of one unmasked statistician.
The primary endpoint was the number of intravitreal ranibizumab injections required over 2 years, tested for superiority (fewer injections). The primary secondary outcome was visual acuity at two years from the Early Treatment of Diabetic Retinopathy Study, tested for non-inferiority (five-letter margin). The primary analysis used the intention-to-treat principle and safety was analyzed per protocol on participants with available data.
The study is registered with ClinicalTrials.gov (NCT02243878) and is closed to recruitment.
Results
411 participants enrolled between January 1, 2015 and December 27, 2019, and 274 were randomly assigned to the 16 Gy SRT group and 137 to the sham SRT group. 240 (58%) of all participants were female and 171 (42%) of all participants were male. 241 participants in the 16 Gy SRT group and 118 participants in the sham group were included in the final analysis, and 409 patients were treated and constituted the safety population, among which two patients assigned to the sham treatment received SRT by mistake 16Gy.
The SRT group received an average of 10.7 injections (SD 6.3) over 2 years versus 13.3 injections (5.8) with simulation, a reduction of 2.9 injections after adjustment for treatment center (CI 95% – 4·2 to –1·6, p<0·0001).
The change in best-corrected visual acuity in the SRT group was not inferior to sham testing (adjusted mean difference in letter loss between groups, –1.7 letters (95% CI –4.2 to 0, 8)). Adverse event rates were similar between groups, but reading center-detected microvascular abnormalities occurred in 77 SRT-treated eyes (35%) and 13 (12%) sham-treated eyes.
Overall, eyes with microvascular abnormalities tended to have better best-corrected visual acuity than those without them. Fewer ranibizumab injections offset the cost of SRT, saving an average of £565 per participant (95% CI – 332 to 1,483).
Interpretation
SRT can reduce the burden of ranibizumab treatment without compromising vision.