Researchers from UCL and Goettingen University Medical Center have created an AI-powered blood test that predicts Parkinson’s disease up to seven years before symptoms appear, using eight biomarkers. This advance, published in Nature Communications, gives hope for early diagnosis and treatment, aimed at protecting brain cells before they are damaged.
A new AI-enhanced blood test can predict Parkinson’s disease up to seven years in advance by analyzing specific biomarkers, potentially enabling earlier and more effective treatments.
A team of researchers, led by scientists from University College of London (UCL) and University Medical Center Goettingen, have developed a simple blood test that uses
” data-gt-translate-attributes=”({“attribute”:”data-cmtooltip”, “format”:”html”})” tabindex=”0″ role=”link”>artificial intelligence (AI) to predict Parkinson’s disease up to seven years before symptom onset.
Parkinson’s disease is the fastest growing neurodegenerative disease in the world, currently affecting nearly 10 million people worldwide.
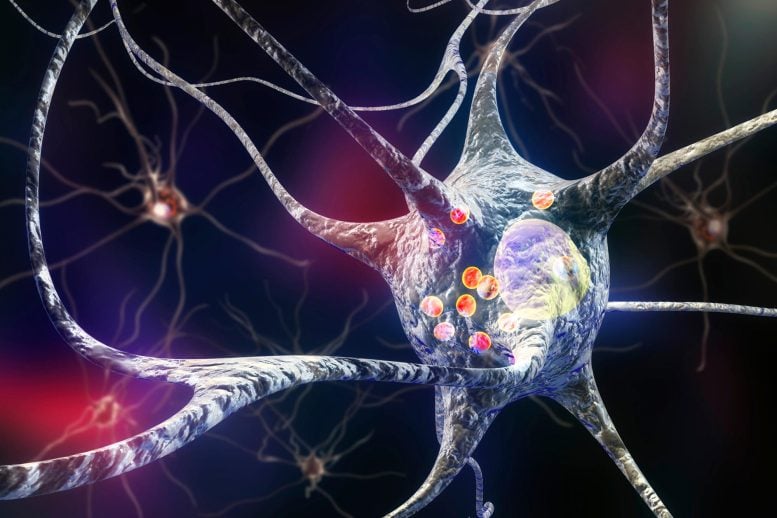
This disease is a progressive disorder caused by the death of nerve cells in the part of the brain called substantia nigra, which controls movement. These nerve cells die or become impaired, losing the ability to produce an important chemical called dopamine, due to the buildup of a protein alpha-synuclein.
Early detection and treatment
Currently, people with Parkinson’s disease are treated with dopamine replacement therapy after they have already developed symptoms, such as tremors, slowness of movement and gait, and memory problems. But researchers believe early prediction and diagnosis would be helpful in finding treatments that could slow or stop Parkinson’s disease by protecting dopamine-producing brain cells.
Lead author Professor Kevin Mills (UCL Great Ormond Street Institute of Child Health) said: “As new treatments become available to treat Parkinson’s disease, we need to diagnose patients before they develop symptoms. We can’t regrow our brain cells, so we need to protect the ones we do have.
“Currently we close the stable door after the horse has run away and we have to start experimental treatments before patients develop symptoms. Therefore, we decided to use cutting-edge technology to find new and better biomarkers for Parkinson’s disease and develop them into a test that we can apply in any major NHS laboratory. With sufficient funding, we hope this will be possible within two years. »
The research, published in
Source link