Researchers at UCSF and UC Davis have discovered a hormone, called Maternal Brain Hormone (CCN3), that maintains bone strength in breastfeeding women despite calcium loss. This hormone could potentially treat osteoporosis and aid in fracture healing in different demographics. The study highlights the importance of including female subjects in biomedical research to uncover gender-specific biological processes.
Researchers at UCSF and UC Davis have identified a new hormone, CCN3, that strengthens the bones of breastfeeding women and could treat osteoporosis and improve fracture healing.
Researchers at UCSF and UC Davis have solved a long-standing mystery about how breastfeeding women maintain strong bones despite losing calcium from milk production.
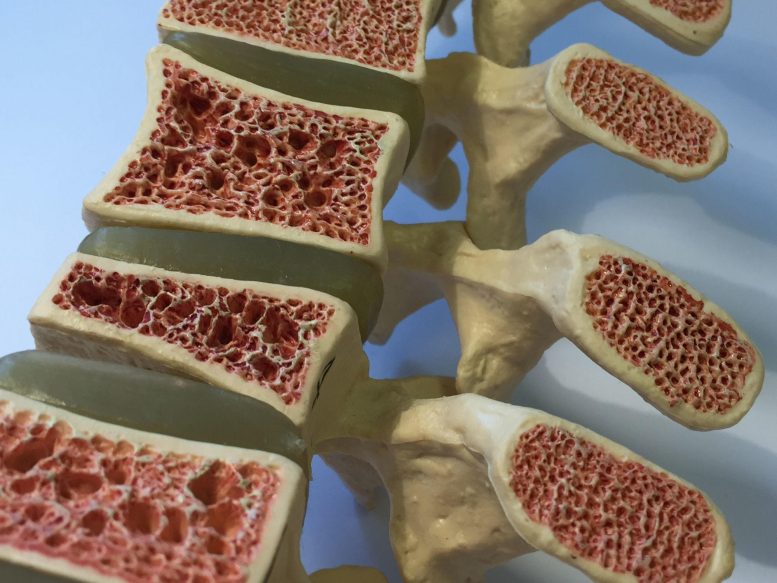
A newly discovered hormone that strengthens the bones of breastfeeding women may also help heal bone fractures and treat osteoporosis in the general population. Researchers at the University of California, San Francisco and the University of California, Davis have shown that in mice, the hormone known as maternal brain hormone (CCN3) increases bone density and strength.
Their results, published in Naturesolve a long-standing puzzle about how women’s bones remain relatively strong during breastfeeding, even when calcium is removed from bones to support milk production.
“One of the remarkable things about these results is that if we hadn’t studied female mice, which is unfortunately the norm in biomedical research, we might have missed this finding entirely,” said Holly Ingraham, PhD, senior author of the new study and professor of cellular and molecular pharmacology at UCSF. “This underscores how important it is to observe both male and female animals throughout their lives to get a complete understanding of biology.”
Osteoporosis and the role of estrogens
More than 200 million people worldwide suffer from osteoporosis, a severe weakening of the bones that can lead to frequent fractures. Women are particularly at risk for osteoporosis after menopause because of the decline in levels of estrogen, a sex hormone that normally promotes bone formation. Estrogen levels are also low during breastfeeding, but osteoporosis and bone fractures are much rarer during this time, suggesting that something other than estrogen is promoting bone growth.
Ingraham’s lab had previously discovered that in female mice, but not male mice, blocking a particular estrogen receptor in certain neurons in a small area of the brain led to a dramatic increase in bone mass. They suspected that a hormone in the blood was responsible for bone strength, but they failed to find it at the time — a search that has continued during the global pandemic.
In the new study, Ingraham and colleagues conducted an exhaustive search for this bone-building hormone and ultimately identified CCN3 as the responsible factor in the mutant females. The team was initially surprised by this result, because CCN3 did not fit the typical profile of a hormone secreted by neurons.
Their doubts were dispelled after they discovered the CCN3 protein in the same brain region in lactating female mice. Without CCN3 production in these selected neurons, the lactating female mice rapidly lost bone mass and their babies began to lose weight, confirming the hormone’s importance in maintaining bone health during lactation. Based on this discovery, they now call CCN3 maternal brain hormone (MBH).
Future CCN3 Testing and Applications
When strategies to increase circulating CCN3 levels were implemented in young and old adult mice, female and male, their bone mass and strength increased dramatically over weeks. In some estrogen-deprived or very old female mice, CCN3 was able to more than double bone mass.
When Ingraham’s scientific collaborator, Thomas Ambrosi, Ph.D., of UC Davis, tested these bones, he was surprised by their strength.
“In some situations, highly mineralized bones are not better; they can be more fragile and break more easily,” he explained. “But when we tested these bones, they were much stronger than usual.”
Ambrosi looked closely at the stem cells in bones that are responsible for generating new bone, and found that when these cells were exposed to CCN3, they were much more likely to generate new bone cells.
To test the hormone’s ability to promote bone healing, the researchers created a hydrogel patch that could be applied directly to the site of a bone fracture, where it would slowly release CCN3 over two weeks. In older mice, bone fractures typically don’t heal well. However, the CCN3 patch stimulated new bone formation at the fracture site, helping the fracture heal more youthfully.
“We’ve never been able to achieve this type of mineralization and healing outcome with any other strategy,” Ambrosi said. “We’re really excited to continue this and potentially apply CCN3 in the context of other problems, such as cartilage regrowth.”
The researchers plan to conduct future studies on the molecular mechanisms of CCN3, its levels in lactating women, as well as the hormone’s potential to treat various bone conditions.
Dr. Muriel Babey, co-senior author and a mentored physician-scientist in the UCSF Division of Endocrinology, is interested in beginning to study the impact of CCN3 on bone metabolism in clinically relevant disease situations. In partnership with the UCSF Catalyst Program, Dr. William Krause, principal scientist and co-leader of this project, will begin to translate these new findings.
“Bone loss occurs not only in postmenopausal women, but also often in breast cancer survivors taking certain hormone blockers, in younger, highly trained elite female athletes, and in older men who have a lower relative survival rate than women after hip fracture,” Ingraham said. “It would be incredibly exciting if CCN3 could increase bone mass in all of these scenarios.”
Reference: “A Maternal Brain Hormone That Builds Bones” by Muriel E. Babey, William C. Krause, Kun Chen, Candice B. Herber, Zsofia Torok, Joni Nikkanen, Ruben Rodriguez, Xiao Zhang, Fernanda Castro-Navarro, Yuting Wang, Erika E. Wheeler, Saul Villeda, J. Kent Leach, Nancy E. Lane, Erica L. Scheller, Charles KF Chan, Thomas H. Ambrosi, and Holly A. Ingraham, July 10, 2024, Nature.
DOI: 10.1038/s41586-024-07634-3
This work was supported by the
” data-gt-translate-attributes=”({“attribute”:”data-cmtooltip”, “format”:”html”})” tabindex=”0″ role=”link”>National Institutes of Health (R01DK121657-S1, NIA-1K01AG065916, 5K12GM081266, K99DK129763, AG066963, R01DK132073, R01AG067740, R01AG070647, R01AG062331, R01DK121657), a Stanford Pilot Award, and a Senior Scholar Award (GCRLE0320).