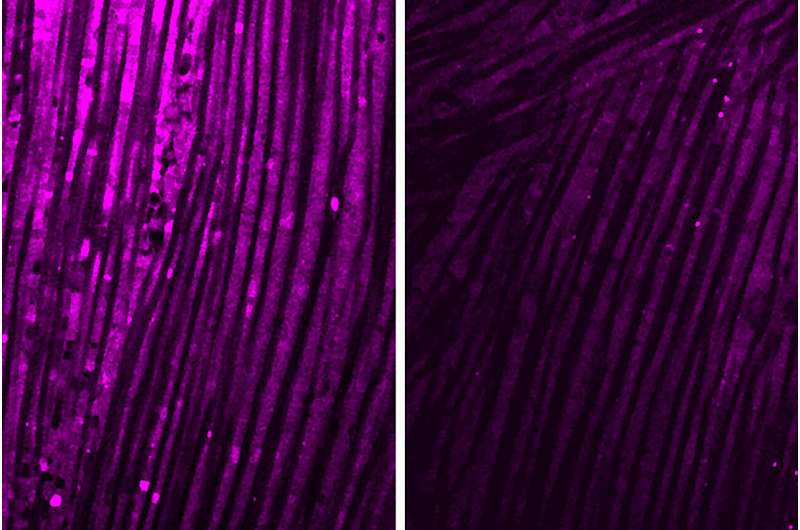
Research from Washington University School of Medicine in St. Louis reveals how brain inflammation triggers extreme muscle weakness in several diseases, including viral infections, bacterial infections, and Alzheimer’s disease. Shown here are fruit fly muscles; the purple coloration is a measure of the ability of muscle cell mitochondria to produce energy. On the left is healthy muscle, and on the right is muscle exposed to IL-6, an immune-related molecule produced by the brain in response to infections or chronic illness. Credit: Shuo Yang
Infections and neurodegenerative diseases cause inflammation in the brain. But for reasons unknown, patients with brain inflammation often develop muscle problems that appear to be independent of the central nervous system. Researchers at Washington University School of Medicine in St. Louis have revealed how brain inflammation releases a specific protein that travels from the brain to the muscles and causes loss of muscle function.
The study, conducted in fruit flies and mice, also identified ways to block this process, which could have implications for treating or preventing muscle wasting sometimes associated with inflammatory diseases, including bacterial infections, Alzheimer’s disease and long COVID.
The study is published July 12 in the journal Scientific immunology.
“We want to understand the very profound muscle fatigue associated with some common diseases,” said lead author Aaron Johnson, Ph.D., associate professor of developmental biology.
“Our study suggests that when we get sick, messenger proteins from the brain circulate in the bloodstream and reduce energy levels in skeletal muscle. It’s not just a lack of motivation to move because we don’t feel well. These processes reduce energy levels in skeletal muscle, thereby decreasing the ability to move and function normally.”
To study the effects of brain inflammation on muscle function, the researchers modeled three different types of diseases: E. coli bacterial infection, SARS-CoV-2 viral infection, and Alzheimer’s disease.
When the brain is exposed to inflammatory proteins characteristic of these diseases, harmful chemicals called reactive oxygen species build up. These reactive oxygen species prompt brain cells to produce an immune-related molecule called interleukin-6 (IL-6), which circulates throughout the body via the bloodstream.
The researchers found that IL-6 in mice, and the corresponding protein in fruit flies, reduced energy production in muscle mitochondria, the cells’ energy factories.
“Flies and mice that had COVID-associated proteins in their brains showed reduced motor function: the flies didn’t climb as well as they should have, and the mice didn’t run as well or as much as control mice,” Johnson said.
“We observed similar effects on muscle function when the brain was exposed to proteins associated with bacteria and the Alzheimer’s disease protein amyloid beta. We also found that this effect can become chronic. Even if an infection is quickly cleared, the decrease in muscle performance persists for several days longer in our experiments.”
Johnson, along with collaborators at the University of Florida and first author Shuo Yang, Ph.D. — who did this work as a postdoctoral researcher in Johnson’s lab — argue that the same processes are likely relevant in people.
Meningitis, a bacterial brain infection, is known to increase IL-6 levels and may be associated with muscle problems in some patients, for example. Among COVID-19 patients, SARS-CoV-2 inflammatory proteins have been found in the brain during autopsy, and many long-COVID patients report extreme fatigue and muscle weakness even long after the initial infection has cleared.
Alzheimer’s disease patients also have increased levels of IL-6 in the blood as well as muscle weakness.
The study identifies potential targets to prevent or treat muscle weakness related to brain inflammation. The researchers found that IL-6 activates what is called the JAK-STAT pathway in muscles, which causes mitochondria to reduce energy production.
Several treatments already approved by the Food and Drug Administration for other diseases can block this pathway. JAK inhibitors as well as several monoclonal antibodies against IL-6 are approved to treat various types of arthritis and manage other inflammatory diseases.
“We don’t know exactly why the brain produces a protein signal that is so damaging to muscle function in so many different disease categories,” Johnson said.
“If we want to speculate about possible reasons why this process has persisted throughout human evolution, despite the damage it causes, it could be a way for the brain to reallocate resources to itself as it fights disease. We need more research to better understand this process and its consequences throughout the body.
“In the meantime, we hope our study will encourage further clinical research into this pathway and determine whether existing treatments that block various parts of it can help the many patients who suffer from this type of debilitating muscle fatigue,” he said.
More information:
Shuo Yang et al., Infection and chronic diseases activate a systemic brain-muscle signaling axis, Sciences Immunology (2024). DOI: 10.1126/sciimmunol.adm7908. www.science.org/doi/10.1126/sciimmunol.adm7908
Provided by Washington University School of Medicine
Quote: Scientists identify possible way to block muscle fatigue in long COVID and other diseases (2024, July 12) retrieved July 14, 2024 from https://medicalxpress.com/news/2024-07-scientists-block-muscle-fatigue-covid.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.