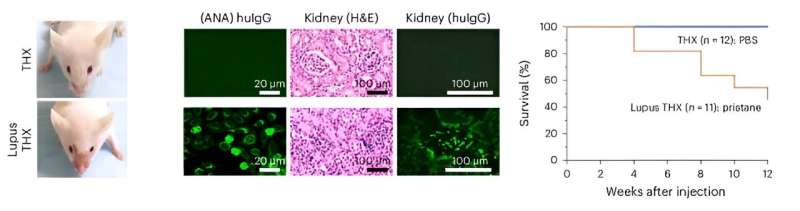
Left, Malar rash in a Lupus THX (huNSGW41 derivative) mouse (three weeks after pristane injection). Middle, Serum antinuclear IgG (scale bar, 20 μm) and renal immunopathology (H&E and anti-huIgG immunofluorescence; scale bar, 100 μm) in Lupus THX and THX mice (12 weeks after pristane or PBS injection). Credit: Natural immunology (2024). DOI: 10.1038/s41590-024-01880-3
A major breakthrough in biomedical research promises new insights into immunotherapy development and disease modeling. Scientists at the University of Texas Health Science Center at San Antonio have created a humanized mouse model with a human immune system and gut microbiome similar to that of humans, capable of producing specific antibody responses.
The scientists were led by Dr. Paolo Casali, the University of Texas Ashbel Smith Professor and Distinguished Research Professor in the Department of Microbiology, Immunology and Molecular Genetics at the Joe R. and Teresa Lozano Long School of Medicine. Casali has five decades of biomedical research experience in immunology and microbiology and is a leading investigator in the molecular genetics and epigenetics of the antibody response.
The goal of the multi-year project, which appears in the August 2024 issue of Natural immunologywas to overcome the limitations of currently available in vivo human models by creating a humanized mouse with a fully developed and functional human immune system.
Mice are widely used in biological and biomedical research because they are small, easy to handle, share many immune elements and biological properties with humans, and are easily genetically modified.
However, many of the more than 1,600 mouse immune response genes are not compatible with their human counterparts, leading to discrepancies or deficiencies in mice as predictors of human immune responses. The availability of a “humanized” mouse model that faithfully reproduces human immune responses has therefore become a top priority.
The first humanized mice were created in the 1980s to model human HIV infection and the human immune response to HIV. Humanized mice were created, and are still created, by injecting immunodeficient mice with human peripheral lymphocytes, hematopoietic stem cells, or other human cells.
However, previous and current models do not develop a fully functional human immune system, have a short lifespan, and do not generate effective immune responses. They are therefore not suitable for the development of in vivo human immunotherapies, modeling of human diseases, or development of human vaccines.
Casali’s team began by injecting immunodeficient NSG W41 mutant mice intracardially (into the left ventricle) with human stem cells that they had purified from umbilical cord blood.
After a few weeks, once the graft is established, the mice are hormonally conditioned with 17b-estradiol (E2), the most potent and abundant form of estrogen in the body. Hormonal conditioning with estrogen was motivated by previous research by Casali and others suggesting that estrogen stimulates the survival of human stem cells, stimulates the differentiation of B lymphocytes and the production of antibodies against viruses and bacteria.
The resulting humanized mice, called TruHuX (for truly human, or THX), have a fully developed and fully functional human immune system, including lymph nodes, germinal centers, human thymic epithelial cells, human T and B cells, memory B cells, and plasma cells that produce highly specific antibodies and autoantibodies identical to those in humans.
THX mice develop mature neutralizing antibody responses against Salmonella Typhimurium and SARS-CoV-2 Spike S1 RBD virus after vaccination with Salmonella flagellin and Pfizer’s COVID-19 mRNA vaccine, respectively. THX mice are also likely to develop full-blown systemic autoimmunity against lupus after injection with pristane, an oil that triggers an inflammatory response.
Casali said the discovery of the THX mouse opens up possibilities for in vivo experimentation in humans, development of immunotherapies such as cancer checkpoint inhibitors, development of human bacterial and viral vaccines, and modeling of many human diseases. He also hopes that this new approach could make the use of nonhuman primates for immunological and microbiological biomedical research obsolete.
Because previous research on the effect of estrogen and the immune system is scarce, Casali hopes this discovery will spur further research on the topic.
“By critically harnessing estrogen activity to support human stem cell and human immune cell differentiation and antibody responses, THX mice provide a platform for studies of the human immune system, human vaccine development and therapeutic product testing,” Casali said.
With the THX model, the Casali lab is now studying the in vivo human immune response to SARS-CoV-2 (COVID-19) at the systemic and local levels, as well as human memory B cells, the dependence on the nuclear receptor RORα for their generation, and the events that lead to RORα expression and dysregulation.
They are also studying the epigenetic factors and mechanisms involved in the generation of human plasma cells, these cellular factories that produce antibodies – literally thousands per second – against bacteria, viruses or cancer cells.
More information:
Daniel P. Chupp et al, A humanized mouse that mounts mature, hypermutated, and class-switched neutralizing antibody responses, Natural immunology (2024). DOI: 10.1038/s41590-024-01880-3
Provided by the University of Texas Health Science Center at San Antonio
Quote: Scientists Create First Mouse Model With Full, Functioning Human Immune System (July 8, 2024) Retrieved July 8, 2024 from https://medicalxpress.com/news/2024-07-scientists-mouse-function-human-immune.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.